Sickle-GAF, looks like there may be hope down the road.
And this is also very exciting for the future of medicine generally.
 news.berkeley.edu
news.berkeley.edu
And this is also very exciting for the future of medicine generally.
FDA approves first test of CRISPR to correct genetic defect causing sickle cell disease - Berkeley News
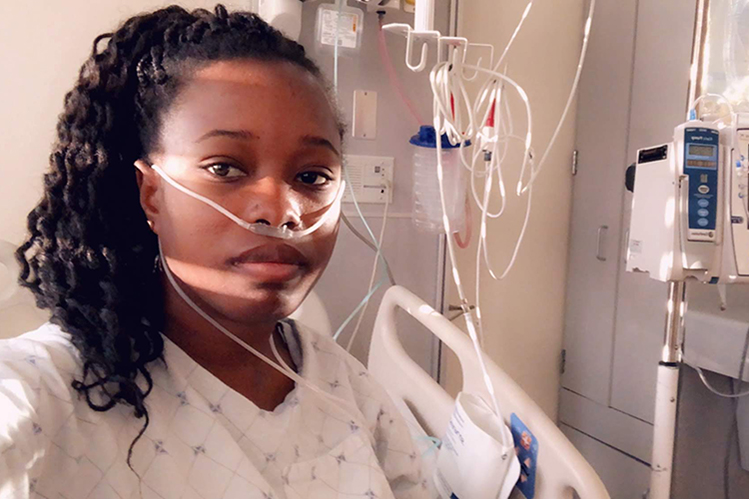
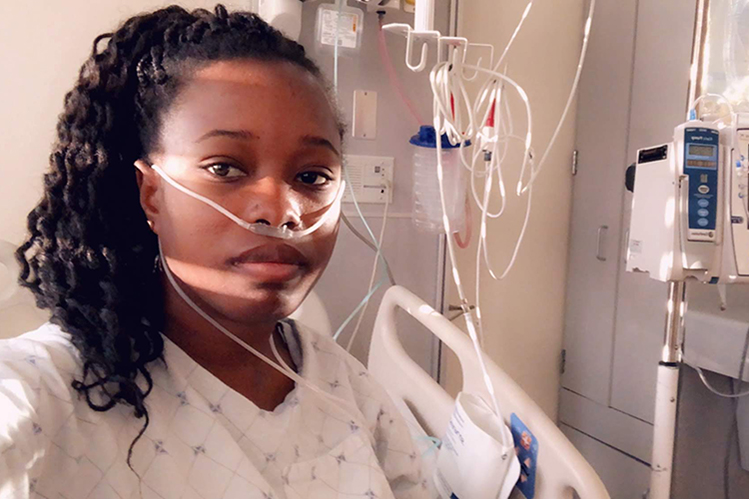
UC scientists and physicians hope to permanently cure patients of sickle cell disease by using CRISPR-Cas9 to replace a defective gene with the normal version
In 2014, two years after her Nobel Prize-winning invention of CRISPR-Cas9 genome editing, Jennifer Doudna thought the technology was mature enough to tackle a cure for a devastating hereditary disorder, sickle cell disease, that afflicts millions of people around the world, most of them of African descent. Some 100,000 Black people in the U.S. are afflicted with the disease.
Mobilizing colleagues in the then-new Innovative Genome Institute (IGI) — a joint research collaboration between the University of California, Berkeley, and UC San Francisco — they sought to repair the single mutation that makes red blood cells warp and clog arteries, causing excruciating pain and often death. Available treatments today typically involve regular transfusions, though bone marrow transplants can cure those who can find a matched donor.
After six years of work, that experimental treatment has now been approved for clinical trials by the U.S. Food and Drug Administration, enabling the first tests in humans of a CRISPR-based therapy to directly correct the mutation in the beta-globin gene responsible for sickle cell disease. Beta-globin is one of the proteins in the hemoglobin complex responsible for carrying oxygen throughout the body.
The trials, which are expected to take four years, will be led by physicians at UCSF Benioff Children's Hospital Oakland and UCLA's Broad Stem Cell Research Center who plan to begin this summer to enroll six adults and three adolescents with severe sickle cell disease.
The IGI's clinical diagnostics laboratory, which was built under Doudna's leadership to provide free COVID-19 testing to the Berkeley community, will play a key role in analytical support for the trial by developing diagnostics to monitor patient well-being and track the efficiency of the treatment.
"We are motivated to work toward a cure that can be accessible and affordable to patients worldwide," said Doudna, UC Berkeley professor of molecular and cell biology and of chemistry and a Howard Hughes Medical Institute investigator. "The launch of this trial is an essential first step on that path."
Other trials have successfully used CRISPR-Cas9 to knock out a gene that suppresses the fetal hemoglobin gene, which is normally turned off in humans. That technique reawakens the fetal gene and, in at least three patients, has alleviated symptoms of sickle cell disease.
The new trial is a gene knock-in: The researchers are using CRISPR-Cas9 to replace the defective beta-globin gene with a repaired version, with the goal of creating normal, adult red blood cells and curing the disorder.
"This therapy has the potential to transform sickle cell disease care by producing an accessible, curative treatment that is safer than the current therapy of stem cell transplant from a bone marrow donor," said Dr. Mark Walters, a professor of pediatrics at UCSF and principal investigator of the clinical trial and gene editing project. "If this is successfully applied in young patients, it has the potential to prevent irreversible complications of the disease."
Another clinical trial also using CRISPR to directly correct the sickle cell mutation, but with a slightly different approach, is planned to begin this year, run by Graphite Bio based on research out of Matthew Porteus' lab at Stanford University.