Rentahamster
Rodent Whores
Nothing happened to him. He's doing the same analysis as always.What in the world happened to Dr. Campbell? The crazy leaps of logic he is taking in this video are quite something to behold.
"Crazy leaps of logic"? "Quite something to behold"? A little hyperbolic, don't you think?
What do you think is more likely? A credible guy who has been very consistent over the last year in his analysis and opinion all of a sudden goes bonkers? Or maybe you just don't like what he's saying?
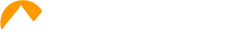
From January 20, 2021 to April 28, 2021 36 (2.6%) of 1,497 observed fully vaccinated healthcare workers tested positive for COVID and 7 (~19%) of those reported persistent symptoms at 6 weeks out in the Israel study he is looking at. So around 20% got "long COVID," which basically matches the general population estimates, yet he strangely decides to twist all of that and instead divide by 1,497 to get a figure of around 0.47%. It makes zero sense to do this, especially when comparing against the widely cited figure that does not use the entire population as the denominator but only those who were infected, because that is the only thing that makes sense.
Makes zero sense? The observed group is 1,497 people. Of those 1,497 people, 7 of them came down with long COVID. i.e. Half a percent of the observed group came down with long COVID. That's a perfectly reasonable interpretation of the data since that's what it literally says.
Can you say that getting vaccinated reduces your chance of getting long COVID? Of course you can. Vaccination already reduces your chances of getting COVID to begin with, so unless the vaccine somehow makes already infected patients have a higher probability of getting long COVID, the vaccination should therefore reduce your overall chances of getting long COVID. Does vaccination somehow make already infected patients more susceptible to long COVID? That's unlikely but at this point unknown.
You're right that a more apples to apples (math wise) comparison would be better, since the 19% from the cited study only includes the infected, which is what the other studies that have long COVID data do. However, I don't know where Campbell is getting his first 10% from that he states in the beginning of the video, so I can't comment on that.
As far as what I know, this is what we know:
Symptom Duration and Risk Factors for Delayed Return to Usual...
Prolonged symptom duration and disability are common in adults hospitalized with severe coronavirus disease 2019 (COVID-19). Characterizing return to baseline health among outpatients with milder...
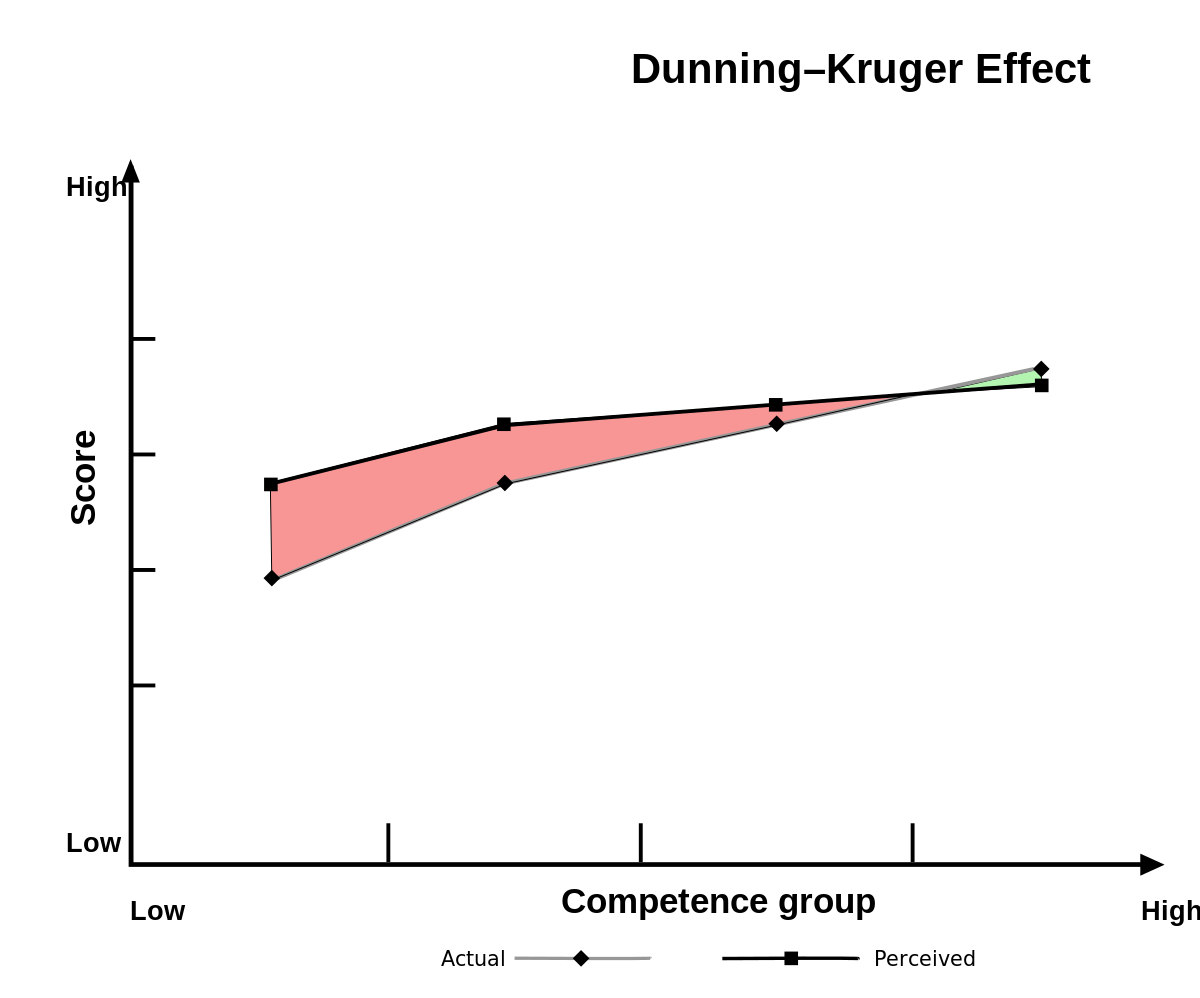
In a multistate telephone survey of symptomatic adults who had a positive outpatient test result for SARS-CoV-2 infection, 35% had not returned to their usual state of health when interviewed 2–3 weeks after testing. Among persons aged 18–34 years with no chronic medical conditions, one in five had not returned to their usual state of health.

Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App
Reports of “Long-COVID”, are rising but little is known about prevalence, risk factors, or whether it is possible to predict a protracted course early in the disease. We analysed data from 4182 incident cases of COVID-19 who logged their symptoms prospectively in the COVID Symptom Study app. 558...
Applying a weighting following the UK population (see Supplementary Methods) the estimated proportion of people experiencing symptomatic COVID-19 going on to suffer long-COVID were similar: 14.5%, 5.1% and 2.2% for 4, 8- and 12-weeks duration respectively. These estimates may still be conservative: whilst estimates could be inflated due to PCR testing in the first wave being restricted to those more severely unwell, or if regular logging may have encouraged more symptoms to be noticed, Long-COVID may here be underestimated if individuals with prolonged symptoms were more likely to stop logging symptoms on the app.

Study Puts Numbers to 'Long COVID' Duration, Prevalence
High frequency of debility lasting for months
Among COVID-19 patients whose infections ranged from asymptomatic to severe, two problems -- fatigue and loss of smell or taste -- persisted most frequently, reported Helen Chu, MD, MPH, of University of Washington in Seattle, and co-authors, in a JAMA Network Open research letter.
"The effects of COVID-19 can linger far beyond acute infection, even in individuals who experienced mild illness," said co-author Denise McCulloch, MD, MPH, also of University of Washington.
"To our knowledge, this study presents the longest follow-up symptom assessment post-illness, with individuals surveyed out to 9 months after their COVID diagnosis," she told MedPage Today.
Earlier studies focused largely on long-term effects in hospitalized COVID patients, McCulloch noted. "Our study is unique in characterizing a group consisting of mostly outpatients: 90% of our cohort experienced only a mild COVID-19 illness, yet one-third continue to have lingering effects," she said.
Early in 2021, researchers in Wuhan, China, reported that 76% of hospitalized COVID-19 patients had at least one symptom that persisted 6 months after acute infection, mostly fatigue or muscle weakness. "Studies of non-hospitalized patients have shown that anywhere from 35% to 50% of non-hospitalized patients had symptoms 2 to 4 months later," Navis noted.

How Common Is ‘Long Covid’? New Studies Suggest More Than Previously Thought
Once upon a time, it seemed that once you recovered from Covid-19, you were home free. Now we know that's not always the case.
 www.forbes.com
www.forbes.com
A survey earlier this month from the Office for National Statistics in Britain polled more than 20,000 participants who'd tested positive for Covid-19 in the last year and found that one in five survivors reported having symptoms after five weeks—and at 12 weeks, the number was still 13.7% (almost one in seven people). The most common symptoms experienced at five weeks were fatigue (11.8%), cough (11%), headache (10%), and muscle pain (7.7%). (Loss of taste and smell followed, each affecting about 6.3% of participants.) At 12 weeks, the prevalence of symptoms was slightly lower, but still distributed similarly and much higher than a control group who hadn't had Covid-19.
In terms of the big picture, when the authors extrapolated the numbers to the whole of the UK, they suggest that more than a million residents may have experienced long Covid by the beginning of March 2021.
This would be the closest comparison to an overall population study, since if we assume a million people in UK had long COVID, and given 68 million UK citizens, that's about a 1.5% prevalence. Still higher than 0.5%. However, these numbers are very imprecise, and should be taken with a large grain of salt since the two populations compared are very different and the involve lots of assumptions.
A study out last week from the Karolinska Institute reported that among a group of healthcare workers who'd had mild Covid-19, 10% still had at least one symptom severe enough to impact their work, home, or social lives eight months later (the most common symptoms were loss of smell and taste, fatigue, and respiratory problems). While the study was quite small and the results should be interpreted with some caution, other studies have also suggested that even mild initial illness can lead to long-term effects.
Can you get long-haul Covid if you're fully vaccinated? Here's what doctors say
It is theoretically possible for a fully vaccinated person to get long Covid. But doctors contend that it doesn't appear to be a significant risk.
Breakthrough infections resulting in long Covid-19 are "quite rare," said Dr. Greg Vanichkachorn, an occupational medicine specialist who works with post-Covid-19 syndrome patients at the Mayo Clinic in Rochester, Minnesota.
Vanichkachorn's observation, while based only on what he's seen in the clinic, is echoed at other post-Covid-19 clinics.
Dr. Michele Longo, an assistant professor of neurology at Tulane University in New Orleans who works with long-haul patients, said she has not seen such patients following a breakthrough infection. Neither has Dr. Maureen Lyons, medical director of the Care and Recovery from Covid-19 Clinic at Washington University in St. Louis.
Dr. Ziyad Al-Aly, a clinical epidemiologist, also at Washington University, is studying the effects of Covid-19 vaccination on the risk of long Covid-19. His research, which is not yet finished, looks at information on more than 5 million veterans within a Department of Veterans Affairs database, including 200,000 who were diagnosed with Covid-19.
"Of the people who get vaccinated and end up with a breakthrough infection, their risk of coming back to the clinic with some long Covid manifestation is very, very small," Al-Aly said.
So, lots of info out there that would suggest it helps.
Furthermore, this is a period of 14 weeks. You can't just take that and declare a percentage of likelihood, especially in light of what happened very soon afterwards in Israel with the Delta variant that we know infects the vaccinated at a vastly higher rate, nevermind any concerns of waning immunity over time.
You can declare a percentage of likelihood, as long as you qualify that it's only within the scope of the study, and acknowledge its limitations, which Campbell did.
No, it really isn't.This is a very strange and extremely misleading video.
Also, there's is preliminary data that show that even post infection, vaccinations could possibly help long haulers.

Are vaccines safe in patients with Long COVID? A prospective observational study
Introduction Although the efficacy of SARS-CoV-2 vaccination to prevent symptomatic COVID-19 is well established, there are no published studies on the impact on symptoms in patients with Long Covid. Anecdotal reports have suggested both a potential benefit and worsening of symptoms post...
Forty-four vaccinated participants were assessed at a median of 32 days (IQR 20-41) post vaccination with 22 matched unvaccinated participants. Most were highly symptomatic of Long Covid at 8 months (82% in both groups had at least 1 persistent symptom), with fatigue (61%), breathlessness (50%) and insomnia (38%) predominating. There was no significant worsening in quality-of-life or mental wellbeing metrics pre versus post vaccination. Nearly two-thirds (n=27) reported transient (<72hr duration) systemic effects (including fever, myalgia and headache).
When compared to matched unvaccinated participants from the same cohort, those who had receive a vaccine had a small overall improvement in Long Covid symptoms, with a decrease in worsening symptoms (5.6% vaccinated vs 14.2% unvaccinated) and increase in symptom resolution (23.2% vaccinated vs 15.4% unvaccinated) (p=0.035).

Mysterious Ailment, Mysterious Relief: Vaccines Help Some COVID Long-Haulers
The possibility that vaccines meant to prevent the disease may also be a treatment for long COVID — when symptoms linger for months — has sparked optimism among patients and scientists.
An estimated 10% to 30% of people who get COVID-19 suffer from lingering symptoms of the disease, or what's known as "long COVID."
Judy Dodd, who lives in New York City, is one of them. She spent nearly a year plagued by headaches, shortness of breath, extreme fatigue and problems with smell, among other symptoms.
Everything changed after she got her COVID-19 vaccine.
"I was like a new person, it was the craziest thing ever," says Dodd, referring to how many of her health problems subsided significantly after her second shot.
And she's not alone. As the U.S. pushes to get people vaccinated, a curious benefit is emerging for those with this post-illness syndrome: Their symptoms are easing and, in some cases, fully resolving after they get vaccinated.
In the absence of large studies, researchers are culling what information they can from patient stories, informal surveys and clinicians' experiences. For instance, about 40% of the 577 long COVID patients contacted by the group Survivor Corps say they felt better after getting vaccinated.
Griffin, who is running a long-term study of post-COVID illness, initially estimated that about 30% to 40% of his patients felt better. Now, he believes the number may be higher, as more patients receive their second dose and see further improvements.
"We've been sort of chipping away at this [long COVID] by treating each symptom," he says. "If it's really true that at least 40% of people have significant recovery with a therapeutic vaccination, then, to date, this is the most effective intervention we have for long COVID."
A small U.K. study, not yet peer-reviewed, found about 23% of long COVID patients had an "increase in symptom resolution" post-vaccination, compared to about 15% of those who were unvaccinated.
But not all clinicians are seeing the same level of improvement.
Clinicians at post-COVID clinics at the University of Washington in Seattle, Oregon Health & Science University in Portland, National Jewish Health in Denver and the University of Pittsburgh Medical Center tell NPR that so far, a small number of patients — or none at all — have reported feeling better after vaccination, but it wasn't a widespread phenomenon.
"I've heard anecdotes of people feeling worse, and you can scientifically come up with an explanation for it going in either direction," says UCSF's Deeks.
Indeed, doctors and online surveys also have found that a smaller fraction of patients say their symptoms worsened after vaccination, although generally doctors continue to advise that those with long COVID get vaccinated to protect against reinfection.