There are ways to measure the viral particles in the air. It's exactly how agencies have measured that aerosolized viral particles can stay in the air for hours. It really should not be a difficult experiment for any facility with the right equipment and it would answer, unequivocally, the effectiveness of different face coverings specifically in regards to COVID-19. If I was faced with undeniable evidence that masks are effective at significantly reducing viral spread and infection, then I would happily jump on the bandwagon and even become an evangelist for wearing them.
It shouldn't be difficult because it's not.
Guidelines from the CDC and the WHO recommend the wearing of face masks to prevent the spread of coronavirus (CoV) disease 2019 (COVID-19); however, the protective efficiency of such masks against airborne transmission of infectious severe acute respiratory syndrome CoV-2 (SARS-CoV-2)...

msphere.asm.org
The potential for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission via infective droplets and aerosols (
1), coupled with guidelines from the CDC (
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/diy-cloth-face-coverings.html) and WHO (
https://www.who.int/emergencies/dis...9/advice-for-public/when-and-how-to-use-masks) recommending the wearing of face masks to prevent the spread of CoV disease 2019 (COVID-19), prompted us to evaluate the protective efficiency of face masks against airborne transmission of infectious SARS-CoV-2 droplets/aerosols.
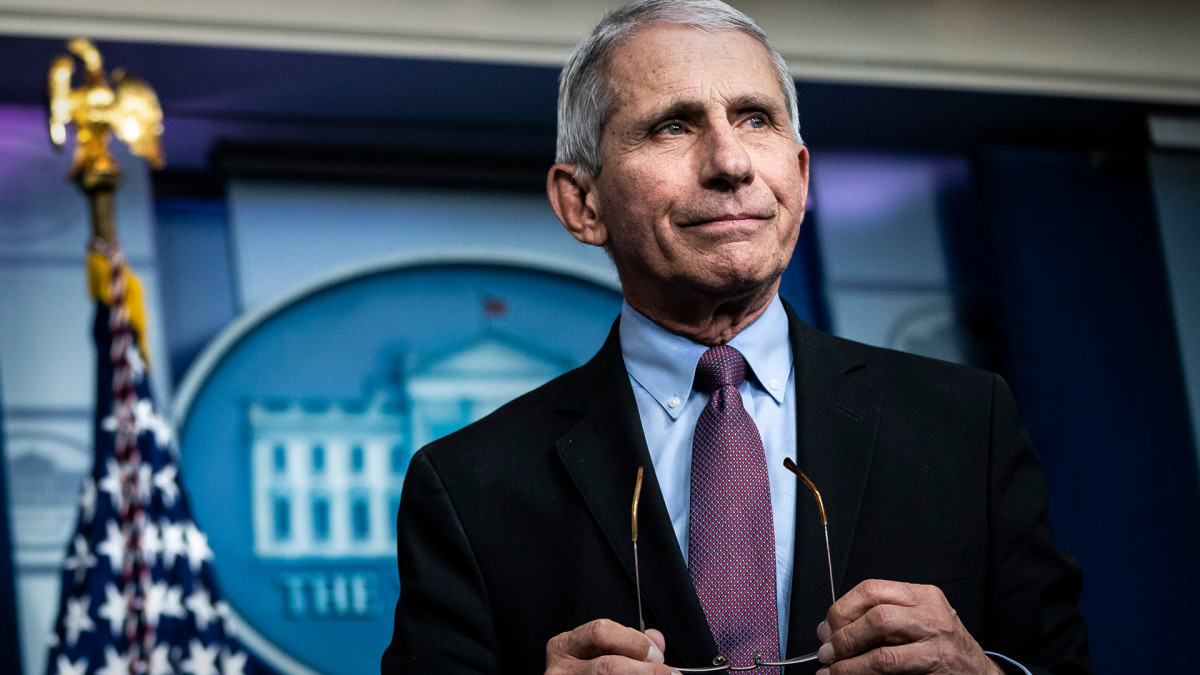
Guidelines from the CDC and the WHO recommend the wearing of face masks to prevent the spread of coronavirus (CoV) disease 2019 (COVID-19); however, the protective efficiency of such masks against airborne transmission of infectious severe acute respiratory syndrome CoV-2 (SARS-CoV-2) droplets/aerosols is unknown. Here, we developed an airborne transmission simulator of infectious SARS-CoV-2-containing droplets/aerosols produced by human respiration and coughs and assessed the transmissibility of the infectious droplets/aerosols and the ability of various types of face masks to block the transmission.
We found that cotton masks, surgical masks, and N95 masks all have a protective effect with respect to the transmission of infective droplets/aerosols of SARS-CoV-2 and that the protective efficiency was higher when masks were worn by a virus spreader. Importantly, medical masks (surgical masks and even N95 masks) were not able to completely block the transmission of virus droplets/aerosols even when completely sealed. Our data will help medical workers understand the proper use and performance of masks and determine whether they need additional equipment to protect themselves from infected patients.
A test chamber for airborne transmission experiments was constructed in a biosafety level 3 (BSL3) facility, and two mannequin heads were placed facing each other. One mannequin head was connected to a customized compressor nebulizer and exhaled a mist of virus suspension through its mouth, mimicking a virus spreader. The nebulizer was charged with 6 ml of virus suspension at the viral doses in culture medium indicated in
Fig. 2 (without fetal calf serum) or diluted in phosphate-buffered saline to generate droplets/aerosols, and the respiration was exhaled continuously, simulating a mild cough at a flow speed of 2 m/s (
2) for 20 min. Although the initial particle size exhaled was 5.5 ± 0.2 μm in mass median diameter (particle size percentages were as follows: <3 μm, 20%; 3 to 5 μm, 40%; >5 to 8 μm, 40% [
3]), some of the droplets likely gradually evaporated and changed to aerosols. Therefore, both droplets and aerosols were likely present in the chamber. The other mannequin head was connected to an artificial ventilator through a virus particle collection unit. Tidal breathing, conducted by the artificial ventilator, was set to a lung ventilation rate representative of a steady state in adults. Face masks were attached to the mannequin heads, and the viral loads and infective virus that passed through the masks were measured by use of a plaque assay and quantitative real-time reverse transcription PCR (qRT-PCR), respectively.
Viral loads in the inhalation droplets/aerosols were inversely proportional to the distance between the virus spreader and the virus receiver; however, infectious virus was detected even 1 m away (
Fig. 2A). The blue bars and the brown bars in the figures show the viral titers and viral RNA copy numbers, respectively. The numbers below each bar show the percentages relative to the leftmost control column values. When a mannequin exposed to the virus was equipped with various masks (cotton mask, surgical mask, or N95 mask), the uptake of the virus droplets/aerosols was reduced. A cotton mask led to an approximately 20% to 40% reduction in virus uptake compared to no mask (
Fig. 2B). The N95 mask had the highest protective efficacy (approximately 80% to 90% reduction) of the various masks examined; however, infectious virus penetration was measurable even when the N95 mask was completely fitted to the face with adhesive tape (
Fig. 2B). In contrast, when a mask was attached to the mannequin that released virus, cotton and surgical masks blocked more than 50% of the virus transmission, whereas the N95 mask showed considerable protective efficacy (
Fig. 2C). There was a synergistic effect when both the virus receiver and virus spreader wore masks (cotton masks or surgical masks) to prevent the transmission of infective droplets/aerosols (
Fig. 2D and
E).
A short news clip about the study:
Alternatively, you can watch these insightful Youtube videos where they replicate experiments that others have done.